Case Study: Empowering Health Care Organizations in Maryland via HDU
Empowering Health Care Organizations to Collect and Submit Digital Quality Measures via Health Data Utility: A Case Study in Maryland
In June of 2022, the Chesapeake Regional Information System for our Patients (CRISP), Maryland's state-designated health data utility (HDU), partnered with the State of Maryland’s Health Services Cost Review Commission (HSCRC) and Medisolv, a leader in quality management software, to become the first state in the country to successfully receive Electronic Clinical Quality Measure (eCQM) data from Maryland hospitals under a new quality reporting mandate.
The partnership developed because of a shared desire to innovate on digital quality measure strategy. Since the decision to partner, HSCRC, CRISP and Medisolv have worked collaboratively to collect hospital eCQMs, broadening reporting requirements as the initiative progresses each year. While the program and partnership has faced challenges, it has also led to increased public health data reporting and transparency to deliver more equitable and efficient care.
Importance of eCQMs
Electronic clinical quality measures (eCQMs) are standardized performance measures that use data electronically extracted from electronic health records (EHR) and/or health information technology (IT) systems to measure the quality of health care provided.[1] Data collection of quality measures such as eCQMs can serve as a marker of quality for hospitals, health systems, and providers to better manage patient care and identify effective care and treatment interventions.
The Centers for Medicare and Medicaid Services (CMS) uses eCQMs in a variety of quality reporting and value-based purchasing programs. In 2016, it became mandatory for eligible hospitals to report data via eCQMs for the Hospital Inpatient Quality Reporting Program[2] and the Medicare Promoting Interoperability Program[3]. In addition, most hospitals are required to submit eCQMs to The Joint Commission as part of its hospital accreditation.
This data transparency helps payers and regulators identify areas to focus limited dollars available for quality improvement, encourages hospitals and clinicians to improve care, and helps consumers make more informed decisions about health care options.
Background on CRISP, Medisolv, and HSCRC Partnership
CRISP is both the state-designated Health Information Exchange (HIE) and a Health Data Utility (HDU). As the state HIE, CRISP organizes and governs organizational and technical processes for the maintenance transmittal, access or disclosure of electronic health care information between or among health care providers or entities through an interoperable system. Building and expanding on these critical HIE capabilities and infrastructure, as an HDU, CRISP collects, aggregates, and analyzes clinical information, public health data, claims data, health administrative and operations data to assist the state in the evaluation of public health interventions and health equity. Additionally, as a key characteristic of HDUs, CRISP maintains and benefits from a diverse and robust governance structure, including multiple committees with a broad array of engaged stakeholders.
CRISP has worked collaboratively with Maryland’s HSCRC for many years to support HSCRC’s various quality programs and payment initiatives. As an independent regulatory agency under Maryland’s Total Cost of Care Model, HSCRC has the authority to hold a portion of hospital revenue at-risk based on specified performance benchmarks.
In 2021, HSCRC approached CRISP with the request to partner in the collection of eCQMs in order to expand its reporting and transparency to the public. The idea behind the initiative was to enable the state to evaluate hospital performance, identify statewide areas for improvement, and incorporate benchmarks into policy development in a timely and consistent manner. Since providers were already accustomed to logging into CRISP to access clinical data, the decision was made to partner with CRISP on data collection to make the process as seamless as possible for hospitals.
As an HDU, CRISP maintains advanced technical infrastructure and services that are designed to serve a wide range of stakeholder needs. It was recognized at the outset that this project required additional technical services that CRISP did not have internally. To better understand the capabilities of potential vendors and in recognizing the importance of identifying leaders in quality reporting and data collection, CRISP, in collaboration with HSCRC, surveyed existing vendors in this space through a Request for Information (RFI). The RFI allowed CRISP to understand existing eCQM vendor capabilities related to several factors, including the below use cases.
- Ability to both collect and transmit eCQMs from hospitals, to the HSCRC on a quarterly basis.
- Knowledge of data collection for Hybrid Hospital-Wide Readmission measures. Vendors were asked to explain their understanding of hybrid measures, their experience in collecting then, and their approach to combining data from multiple data input streams.
- Knowledge of physician-focused eCQMs for a potential project with another state agency at a later date.
Medisolv was selected as a partner given the company’s leadership in quality management software and its location in Maryland, providing the company with a deep understanding of the Maryland model and its structure.
Early in the project, the Maryland Health Care Commission (MHCC) became actively engaged as a fourth member of this partnership. MHCC is the state regulator that designates CRISP as the state HIE and HDU. MHCC uses the year-end data collected and publishes components of it on their consumer-facing website. This data informs consumers on critical aspects of patient care and population health including patient engagement, safety, prescribed medications, and treatment outcomes.
Reporting Requirements
Since June 2022, HSCRC, MHCC, CRISP and Medisolv have worked collaboratively to collect hospital eCQMs, making Maryland the first state in the country to successfully receive eCQM data from hospitals under a new quality reporting mandate. As of 2022, and under the State of Maryland initiative, hospitals are required to submit quality performance data, independent of CMS reporting requirements, on a quarterly basis via the Medisolv Submission Portal integrated with CRISP’s HIE portal.
At the onset of the initiative, hospitals were required to submit four measures quarterly, with the first submission window opening in July 2022. Data is reported/submitted via the QRDA I that is uploaded to Medisolv via the CRISP HIE portal.
For the 2023 data collection efforts, HSCRC required submission of the Core Clinical Data Elements (CCDE) for hybrid measure. The two hybrid measures that were required include:
- Hybrid HWR: Hospital-Wide 30-day Readmission
- Hybrid HWR: Hospital-Wide 30-day All-Cause Risk Standardized Mortality Measure
Regarding the eCQM measure submission requirements for CY 2024, HSCRC requires submission of QRDA I files for the eCQM’s listed below.
- eOPI-1: Safe Use of Opioids-Concurrent prescribing
- PC-02: Cesarean Birth
- PC-07: Severe Obstetric Complications (risk-adjusted)
- HH-01: Hospital Harm- Severe Hypoglycemia
- HH-02: Hospital Harm- Severe Hyperglycemia
- Two additional eCQM measures of the hospital’s choosing
Measures for 2025 will remain unchanged from 2024, but HSCRC is offering additional flexibility with reporting timelines. Hospitals that do report all the data requested by the deadline will be eligible for a $150,000 bonus per hospital.
Challenges
Until recently, emergency department (ED) utilization was an eCQM (ED-2 measure) that was tracked and required for reporting by CMS. Given that the measure is no longer required by CMS, vendors decided to stop reporting this measure and additionally, stopped supporting the specifications related to ED wait times. As a result, HSCRC removed reporting requirements for ED utilization and instead set up a separate workgroup, the ED Wait Time Reduction Commission, that focuses on high throughput times in Maryland hospitals, where the backlogs are, and how wait times can be improved.
Additionally, throughout the program, hospitals have occasionally needed to file extension requests for submitting eCQMs to HSCRC. These extension requests, known as Extraordinary Circumstance Exceptions (ECEs) can be filed with the HSCRC for various reasons, including cyber-attacks and delays in EHR upgrades.
Having the right partnership in place to address these challenges has proved to be of invaluable significance. As an HDU, CRISP has been able to support this program in a neutral and flexible way to ensure goals are met by regularly and frequently communicating with HSCRC, MHCC, and Medisolv to determine how to best support hospitals that have not submitted data and troubleshoot any issues hospitals are reporting.
Significance of Partnership and Benefit to Public Health
In July 2024, MHCC reported the opioid measure for 2023 on their public-facing website and are currently exploring the feasibility of reporting maternal morbidity measures that would be part of a birthing score card for hospitals in Maryland. In 2025, MHCC has decided to publish hyper- and hypo-glycemia measures that were reported for 2024 to provide transparency on treatment outcomes for individuals with diabetes and other related conditions. The partnership between CRISP, HSCRC, MHCC and Medisolv demonstrates state government ability to collect eCQM data to evaluate and advance care quality. Through this work, CRISP, has been able to demonstrate an emerging HDU capability in collecting and submitting quality metrics.
[1] “Electronic Clinical Quality Measures Basics”. Centers for Medicare & Medicaid Services. September 2024. Available: https://www.cms.gov/medicare/regulations-guidance/promoting-interoperability-programs/electronic-clinical-quality-measures-basics#:~:text=Health%20care%20providers%20are%20required,to%20measure%20health%20care%20quality.
[2] “Hospital Inpatient Quality Reporting Program”. Centers for Medicare & Medicaid Services. September 10, 2024. Available: https://www.cms.gov/medicare/quality/initiatives/hospital-quality-initiative/inpatient-reporting-program
[3] “2022 Medicare Promoting Interoperability Program Requirements”. Centers for Medicare & Medicaid Services. September 24, 2024. Available: https://www.cms.gov/2022-medicare-promoting-interoperability-program-requirements
March 2025 Network News
March Network News
Thank you to everyone who joined us for the March 2025 Network News where we heard from Kevin McAvey about proposed Medicaid funding cuts and their far-reaching implications. We covered:
- how these funding changes could impact your organization
- Civitas’ advocacy efforts and next steps in response to the proposed cuts
- perspectives, questions, and concerns from Civitas members
If you want a refresher or if you couldn’t make it to the live event, please check out the recording and presentation slides linked below.
How CareQuest Institute for Oral Health is Transforming Oral Health

CareQuest Institute for Oral Health is committed to making oral health more accessible, equitable, and integrated. Guided by a mission to improve the oral health of all, the Institute addresses systemic disparities through strategic innovation, partnerships, and evidence-based programs. From advocating in our nation’s capital to on-the-ground training in local health centers, CareQuest Institute ensures underserved communities receive the care they need.

Advancing Oral Health Through Philanthropy and Community-Driven Solutions
Philanthropy is a cornerstone of CareQuest Institute’s work. By funding and elevating local solutions and addressing structural barriers to oral health access, the Institute helps create healthier communities. Every year, dozens of grantees oversee initiatives that improve health and racial equity, strengthen community partnerships, and drive policy change.
Within the Institute’s philanthropic efforts, the Oral Health Progress and Equity Network (OPEN) amplifies community voices in policy advocacy. OPEN enables the Institute to align with community-driven oral health priorities and engage in strategic advocacy.
CareQuest Institute’s policy and advocacy team collaborates with policymakers, advocacy groups, and coalitions to ensure oral health is a priority at the state and national levels. In 2024, that work was displayed in the U.S. Senate, as leaders advocated for the inclusion of oral health in Medicaid adult dental benefits and explored integrated care reimbursement models.
This multi-pronged philanthropic and advocacy approach helps ensure that oral health remains a priority at all levels of government.

Overcoming Challenges in Oral Health Care
Despite progress, challenges persist in achieving equitable oral health access, including:
- Disparities in care access
- Lack of medical-dental integration
- Gaps in dental coverage, particularly within Medicaid and Medicare
- Health IT barriers, including limited data-sharing capabilities in dental software
- Workforce shortages

CareQuest Institute works to strengthen dental benefits, champion medical-dental integration, and promote the implementation of interoperable dental software. The Institute also offers education through online courses and webinars to empower providers in delivering patient-centered and equitable care.
Key Reports and Successful Initiatives
CareQuest Institute leverages data to drive transformative change. Through research, surveys, and reports, the Institute uncovers trends and informs policy decisions. Some key initiatives include:
- State of Oral Health Equity in America Report: Provides an annual national analysis of oral health experiences and behaviors to influence policy and community empowerment.
- Oral Health Progress and Equity Network (OPEN): Explore the Equity Network Toolkit and theElection Engagement Toolkit for resources on advocacy and community engagement.
- A Simple Alternative Payment Model (APM) for Diabetes and Periodontal Care: Highlights how integrating periodontal treatment into diabetes management improves outcomes and reduces costs.
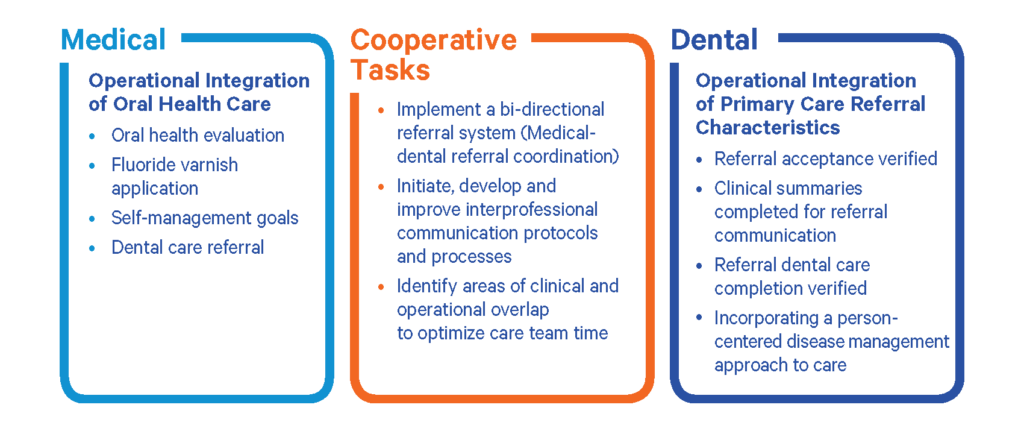
Diving Deeper: Bridging Gaps with the MORE Care® Program
Focused on bridging the gap between medical and dental practices, MORE Care® (Medical Oral Expanded Care) is a program that integrates oral health into comprehensive, person-centered care. From 2022 to 2024, the program was implemented in Ohio, building sustainable networks that improved referral processes and access to oral health services.
Despite challenges like the lack of integrated electronic records necessitating manual referral tracking, the program successfully referred 407 patients from primary care to dental practices, achieving 100% growth in referrals over the baseline. This success reflects the importance of referral relationships yet underscores the need for streamlined, interoperable systems to support medical-dental collaboration and improve care access.
Community Oral Health Transformation (COrHT), another program of the CareQuest Institute, recently helped grow integrated care models across 13 safety net dental clinics across North Carolina. The program operated in partnership with the NC Oral Health Collaborative and BlueCross BlueShield of NC Foundation.
While COrHT NC participants collected and utilized oral health data within their value-based care models, the lack of standardized data exchange limited full integration with medical systems.
CareQuest Institute and their partners encounter the critical need for dental data standardization frequently. Civitas Networks for Health and its members play a vital role in advocating for improved health information sharing and advancing policies that support provision of comprehensive care, including oral health.
Building Strategic Partnerships for Systemic Change
Collaboration is integral to CareQuest Institute’s focus on driving oral health transformation. By partnering with organizations like Civitas, HL7, the Workgroup for Electronic Data Interchange (WEDI), and other mission-aligned entities, the Institute enhances data exchange standards and expands oral health data analytics, improving interoperability and care coordination.
A key example is CareQuest Institute’s participation in HL7’s data exchange forum, which promotes standardized integration between health care and dental systems.
By partnering with HL7, CareQuest Institute is advancing efforts to align oral health data with medical standards, ensuring that future initiatives in value-based care fully integrate oral health into comprehensive patient care.

Joining Civitas Networks for Health: A Strategic Partnership for Broader Impact
Three years ago, CareQuest Institute joined Civitas Networks for Health to further elevate our work in oral health integration with the national platform for advancing health information exchange, interoperability, and data governance. We appreciate the connection to a robust network of health data organizations and regional health information exchanges, allowing CareQuest Institute to advocate for integrated health data systems that include oral health.
“This partnership enables CareQuest to engage in policy discussions at a national level, advocating for inclusive data standards, and collaborating on innovative solutions to expand oral health data analytics,” said Andrea Clark at CareQuest Institute for Oral Health.
This collaboration strengthens CareQuest Institute’s efforts to:
- Expand technology-driven solutions for integrated care
- Improve health care workflows through innovative systems
- Promote health IT education to enhance data interoperability
- Advance value-based care models
CareQuest Institute’s Future Vision and Goals
Success for CareQuest Institute means helping to create a health care system where oral health is a fundamental right, not a privilege. This vision is measured by better access to care within communities and improved oral health outcomes.
To learn more about their wide array of tools, reports, and resources, check out the CareQuest Resource Library.

FHIR Webinar Series - Session 5: CARIN Alliance
In this fifth meeting of the FHIR Deep Dive Webinar Series, we heard from the CARIN Alliance. Watch the recording below.
Meet the Inaugural Civitas Networks for Health Government Relations and Advocacy Committee
Civitas is thrilled to introduce our first-ever Government Relations and Advocacy Committee (GRAC), chaired by Civitas Board member, Craig Behm, President and CEO of CRISP - Chesapeake Regional Information System for our Patients. This dynamic group represents a diverse array of Civitas full and affiliate members, each bringing extensive federal and state government relations experience to the table.
The GRAC will play a pivotal role in shaping and executing Civitas’ public policy agenda, focusing on key priorities including interoperability, quality improvement, data infrastructure, and human service integration. By leveraging their extensive experience and organizational influence, GRAC members will drive strategic impact, enhance communication with the Board of Directors, and provide valuable guidance to Civitas members throughout this busy legislative year.
Meet Our GRAC Members:
- Angie Bass, Velatura Public Benefit Corporation
- Alisa Kuehn, Indiana Health Information Exchange
- Bethany Hall, Quality Insights
- Chinonye Onwunli, Blue Cross Blue Shield Association
- Eliel Oliveira, Connxus
- Felix Su, Manifest MedEx
- Jacqueline Welsch, HEALTHeLINK
- Jane Pederson, Stratis Health
- Jaime Bland, CyncHealth
- Jenelle Hoseus, Health Impact Ohio
- Karen Johnson, American Academy of Family Physicians
- Kyle Russell, Virginia Health Information
- Lindsey Wisham, Telligen
- Martin Ciccocioppo, PA eHealth Partnership Program, OMAP, DHS
- Melissa Breen, Wisconsin Collaborative for Healthcare Quality
- Neil Sarkar, Rhode Island Quality Institute
- Phil Ennen, The Ohio Health Information Partnership
- Robin Ford, New Jersey Innovation Institute
- Scott Bennett, Contexture
- Sonia Chambers, West Virginia Health Information Network
- Terri Stewart, SYNCRONYS
- Will Battles, Alliant Health Solutions
Congratulations to our inaugural GRAC members! We are excited to see the impact of your leadership and vision on health policy and advocacy.
Member Webinar | J2 Interactive: How Top HIEs are Using Salesforce to Grow Webinar Featuring KONZA
Member Webinar | J2 Interactive: How Top HIEs are Using Salesforce to Grow Webinar Featuring KONZA
Thank you to all who joined us for an insightful webinar from Civitas Member J2 Interactive on February 27, 2025. This discussion shared insights on how HIEs from around the country are utilizing SalesForce to Grow and featured insights from KONZA National Network.
Questions? Please reach out to contact@civitasforhealth.org.
Ohio’s Community Health Workers and Their Impact on Vulnerable Populations
Community Health Workers (CHWs) play a critical role in addressing social determinants of health and improving health outcomes for vulnerable populations. By acting as trusted advocates and navigators, CHWs bridge the gap between individuals and the often-complex health care system. Through innovative models, legislative support, and dedicated training programs, Ohio is paving the way for a more effective and equitable approach to care delivery.
This topic was explored in depth during the Civitas Networks for Health Annual Conference in October 2024, in a session led by Jenelle Hoseus, a Civitas board member and Chief Policy and Partnerships Officer for Health Impact Ohio, and Chief Executive Officer for Central Ohio Pathways HUB, alongside Tanikka Price, Chief Education & Equity Officer for Health Impact Ohio.
Their presentation highlighted Ohio’s innovative strategies to support CHWs and the communities they serve.
Background on Health Impact Ohio
Health Impact Ohio (HIO), a Regional Healthcare Improvement Collaborative based in Columbus, Ohio and a Civitas member for many years, is committed to advancing equitable health outcomes statewide. Guided by its vision of optimal health for all, HIO tackles social determinants of health, enhances care quality, and improves access through community-driven initiatives.
With a focus on community engagement, training, data integration, and strategic planning, HIO leads impactful programs such as the Central Ohio Pathways HUB and the CHW Certification Program. Supported by partners like the Ohio Department of Health, CDC, and managed care organizations, HIO empowers communities with sustainable solutions to reduce health disparities and improve lives.
What is the Central Ohio Pathways HUB?
The Central Ohio Pathways HUB, created and managed by Health Impact Ohio since 2019, is a care coordination program designed to connect Central Ohio’s most at-risk populations with critical health services and resources. Operating across Franklin, Delaware, Union, Madison, Pickaway, Licking, Marion, Ross, and Fairfield counties, the HUB collaborates with ten Care Coordination Agencies (CCAs) employing 40 CHWs to deliver personalized care and support.
The HUB prioritizes addressing social determinants of health by bridging gaps in:
- Health care access
- Social support services
- Community resource connections
How the HUB Works
 Image Source: Health Impact Ohio
Image Source: Health Impact Ohio
Together, the Central Ohio Pathways HUB and its partners are driving better health outcomes and advancing equity for the region’s most underserved communities.
A Growing Framework: Training for Community Health Workers
Ohio has made significant strides in formalizing and supporting the CHW workforce. The Ohio Board of Nursing oversees CHW certification, ensuring that CHWs receive the training and tools they need to thrive. Certification involves comprehensive training programs and practicum placements, often hosted at the CHW’s place of employment. This structure not only professionalizes the CHW role but also equips these trusted community members with enhanced skills to support families and individuals navigating their health care needs. HIO’s team, led by Dr. Price, has been teaching a CHW Certification course for five years with curriculum that is prenatal care to end of life planning, with a goal of giving constructive education so that CHWs are able to meet the need of any client they may engage with in the future.
To expand opportunities for CHWs, Ohio has introduced programs targeting high school students, creating a pipeline for the next generation of CHWs. Additionally, the Ohio Department of Health has established a Center of Excellence for the CHW model and is developing training programs for CHW supervisors to ensure sustained support and leadership development.
Legislative Support and Sustainability
Ohio’s legislative framework has been instrumental in advancing the CHW model. Senate Bill 332 provided critical policy support to decrease infant mortality, enhanced CHW certification processes, and enabled reimbursement through Medicaid and Managed Care Plans (MCOs). This legislative action, coupled with significant financial support from the Ohio Commission on Minority Health (OCMH), allowed Ohio to grow its Community Care Hub (CCH) model from four to twelve hubs, providing a clear path to sustainability.
Under this model, CHWs partner with MCOs to conduct risk assessments, develop personalized care plans (called “pathways”), and connect clients to essential community resources. This approach has yielded impressive results, including 122 healthy birthweight babies, with 96% born at a healthy weight as seen in HIO’s OCMH data from 2022.
How Community Health Workers Serves as Trusted Partners in Health and Wellbeing
Ohio’s CHWs are more than health care navigators—they are trusted community members dedicated to addressing gaps in access to quality care and services. Demographically diverse, CHWs in Ohio are often driven by a personal passion for improving the well-being of their neighbors. Nearly 90% of CHWs educate individuals and families, and 90% connect clients to vital community resources, demonstrating their critical role in addressing social determinants of health.
Health Impact Ohio has been leading efforts with tens of other Community Based Organizations (CBOs) across the State to focus on how to create standardization in workflows, outcomes data, and eventually reimbursement for community-based interventions, especially those performed by a CHW. This is critical in recognizing CHWs as part of the larger healthcare eco system and to provide services to individuals in a way that is meaningful and meets them where they are.
These initiatives aim to enhance the impact of CHWs while ensuring sustainable funding and operational support.
The Future of Community Health Workers in Ohio
Ohio’s investment in training for community health workers and its innovative HUB model have positioned the state as a leader in leveraging CHWs to address social determinants of health. By aligning legislative support, standardized processes, and community-focused initiatives, Ohio is empowering CHWs to make a lasting impact on vulnerable populations.
As emphasized by Jenelle and Tanikka during their presentation at the Civitas Networks for Health Annual Conference, Ohio’s approach offers valuable lessons for states nationwide. By fostering trust and collaboration at the community level, CHWs are driving health equity and creating a more effective and sustainable health care ecosystem.
Health Data Utility as Public Health Capability: Arkansas SHARE Case Study
By Alan Katz, Associate Director of Advocacy & Public Policy, Civitas Networks for Health
ABSTRACT—Over the past decade, a combination of federal, state, and private-sector investment has rapidly transitioned Arkansas’ health data infrastructure from legacy paper formats to electronic health record (EHR) platforms now present in over 90% of outpatient physician practices and 96% of the acute care hospitals in the state. To help manage and further advance this transition in public interest, the Arkansas State Health Alliance for Records Exchange (SHARE) was established as the state’s official health information exchange (HIE) by a 2011 statute. Now under the Arkansas Department of Health, SHARE has steadily worked to broaden its statewide capabilities beyond point-to-point clinical data sharing to reduce barriers within and between public health agencies to maximize efficiency and improve outcomes. In doing so, it has become one of the nation’s leading functional examples of the health data utility (HDU) model.
__________________
In 2011, the Arkansas legislature created the Arkansas Office of Health Information Technology (OHIT) with a mission to “obtain the maximum potential value from the investment of federal and state resources to increase the use of health information technology” and to further “the coordination of health information technology throughout Arkansas.”[1] The same legislation established Arkansas State Health Alliance for Records Exchange (SHARE) as the state’s official health information exchange for “effective communication…among hospitals, payers, employers, pharmacies, laboratories, and other health care entities” that creates “the ability to monitor community health status” and realize “efficiencies in health care costs.” [2] A year after the bill became law, SHARE launched the original version of its direct messaging service for providers, and a few months later, SHARE’s clinical records platform had its first major partner in North Arkansas Regional Medical Center (NARMC).
Today, NARMC is one of 118 hospitals statewide that participate in SHARE’s network alongside over 3,400 other clinical facilities contributing data and more than 900 facilities receiving data.[3] The information is contributed, processed, and received in the form of dozens of deliverables and analytic products across SHARE’s portfolio. The primary HIE platform incorporates a virtual health record (VHR), direct secure messaging, public health reporting to include (bi-directional immunization reporting, electronic lab reporting (ELR), syndromic surveillance reporting, cancer registry and electronic case reporting (eCR) health plan clinical data delivery, admission-discharge-transfer (ADT) and hospital readmission notifications, Foster Care custody change reports, and laboratory reports, among other functions. Hospitalization reports and continuity of care documentation (CCD) services also exist as independent options. From a baseline of just under a quarter of Arkansas’ office-based physicians who had adopted at least a simple EHR system in 2011[4], SHARE, in concert with the HITECH Act’s meaningful use incentive payments, has helped catalyze and consolidate a system in which over 90% of office-based physicians have done so.[5]
These services are developed and implemented through SHARE’s extensive technology partnerships with the private sector in Arkansas and beyond. This has created a unique and dynamic outlet for health IT innovation that ensures modern technologies and applications can be rapidly integrated into the state’s health system for the benefit of providers, patients, and other stakeholders. SHARE likewise works closely with public sector authorities outside OHIT to improve health IT access and efficiency for essential services, including a longstanding integration with Arkansas Medicaid. In addition SHARE works with Commercial Health Plans, Arkansas PASSE’s – Provider-Led Arkansas Shared Savings Entities, the University of Arkansas for Medical Sciences (UAMS), Arkansas Department of Corrections, and the Arkansas Department of Health (ADH), while having connections to all 94 of the state’s county-based Local Health Units.[6] Additionally, OHIT has partnered with the UUAMS Biomedical Informatics Department to allow fellows to rotate through SHARE to understand health information exchange and interoperability efforts happening statewide. Each fellow rotates for a four-week period and can select an additional rotation as an election in the fellowship.
SHARE has demonstrated considerable progress towards interoperability through its scale and scope of operations. As the network continues to grow and evolve, a key question is whether the HIE label is still the best structural paradigm for SHARE—or whether the complex, multi-layered and blended public-private infrastructure that SHARE maintains is better understood as something newer. How providers, payers, patients, and policymakers conceptualize the fundamental role of the statewide health data system is critical to how it operates and to whom it is ultimately responsible.
Consistent with nationwide trends in expanding public and nonprofit HIE capabilities, SHARE is best characterized as an emerging health data utility (HDU) by virtue of its central governance position for multiple overlapping health data use cases in the state and its role as an accessible resource at the community level across Arkansas.[7] The functional transformation from HIE to HDU is most evident in the broader public health space, where recent SHARE initiatives are focused on leveraging its broad reach and technical depth to keep driving systemic modernization at Arkansas’ public health authorities (PHAs) and strengthening their linkages to SHARE at the same time.
Several items within SHARE’s public health portfolio represent this functional transformation from HIE to HDU. Externally, SHARE provides ADH’s exclusive connection to the eHealth Exchange national network, which among other services gives SHARE access to the Association of Public Health Laboratories (APHL) Informatics Messaging Services (AIMS). Participation in a national network while maintaining local trust networks is just one of many key characteristics of emerging HDUs. AIMS is the nation’s premier information exchange network for public health labs, including ADH’s Baker Public Health Lab, and connects to the Centers for Disease Control and Prevention (CDC) and Arkansas hospitals on AIMS that also contribute data to SHARE. Operationally, this means that SHARE is interposed between these entities and AIMS and consequently has responsibility for ensuring the “data hygiene” and standards compliance of electronic lab reports that flow out from Arkansas to the AIMS network—and to the CDC’s National Syndromic Surveillance System.
SHARE’s position at this central nexus between providers and public health authorities has also made it the de factostate “utility” for ongoing digitization efforts and related systemic upgrades. No less than 70 different EMR platforms statewide currently exchange data with SHARE, each of which must be able to seamlessly connect to the network for their respective facilities and organizations to reap the benefits of interoperability. Lack of fully-standardized data elements and diverse technical specifications are persistent barriers—but in many cases (especially public sector use cases), the SHARE team starts from a lack of any data elements whatsoever. Newborn screening at the hospital (the “heel spot” blood test) is a foundational public health service for identifying a wide range of congenital conditions early, and by 2021 ADH had achieved a 98% screening rate for the 31 conditions tested.[8] The problem to date is that all those lab results have been transmitted via fax, limiting their integration with the rest of ADH’s health information, the national networks, and SHARE’s own systems. Similarly, prior to 2023, a large segment of the agency’s 26 disease registries[9] and associated information were partially or fully running on paper or otherwise unconnected, requiring providers to fax or call in required disease reporting information. For EMS responders seeking to collect and upload data to a central HIE platform, no mechanism exists at all.
Since the end of the COVID-19 pandemic, SHARE has moved quickly and intently to address each of these significant gaps in the system. Working in close collaboration with ADH as well as several of the state’s leading hospital systems[10], registries for infectious disease, maternal mortality, birth defects, traumatic brain injury, and other conditions have been digitized and linked to core components of SHARE’s virtual health record (VHR) and HIE platform infrastructure. Other registries that are already electronic—those for electronic laboratory reporting (ELR), cancer registry, syndromic surveillance, and immunization reporting—are being streamlined through SHARE integration with an emphasis on reducing interfaces which in turn saves the healthcare entities money and time. Applying best practices that were scaled rapidly during the COVID-19 pandemic, the system allows state epidemiologists and Local Health Unit staff to seamlessly access data that includes real-time tracking, demographic information, and monthly updates.
In late 2024, SHARE began piloting the transition from fax machines to electronic lab reports for newborn screening with Arkansas Children’s Hospital, its Epic EHR provider, and the Arkansas Public Health Lab. The initiative is currently finishing its “test monitoring phase” and preparing to go live this year; shortly thereafter, the SHARE team expects to expand the work to other hospitals on the Epic system followed by hospitals contracting with other vendors. At the same time, SHARE is building the state’s first digital platform for real-time EMS data integration with providers through its own infrastructure. The new service has begun in the trial stage as a partnership between ADH, SHARE, and several private ambulance providers to combine alerts, access to continuity of care documents (CCDs), and other parts of the SHARE portfolio centered on its MPI and eCR capabilities. Enabling consolidated reports on patients who were transported and treated in EDs or as inpatients vs those who were not transported after an EMS call will be particularly valuable for primary care follow-up and coordination—which will also be facilitated by SHARE’s HIE platform.
SHARE has also made a priority of continuing to deepen connections between state agencies and sub-agencies that manage health and health-related data as a matter of government and network efficiency, modeling HDUs’ role as key arbiters within the public health enterprise. Among the foremost recent examples of this imperative is its project to integrate beneficiary data from the Special Supplemental Nutrition Program for Women, Infants, & Children (WIC) into other clinical and non-clinical data streams under different divisions of ADH, particularly Medicaid. WIC is administered at the federal level by the USDA’s Food and Nutrition Service, while ADH manages the funding for the state and county Local Health Units deliver the program benefits (healthy food, breastfeeding and nutrition support, and care referrals). Pregnant and postpartum women and young children are automatically eligible if they are already enrolled in Medicaid or SNAP.[11]
Despite this large pool of potential beneficiaries, only 53.5% of eligible people nationwide are enrolled in WIC[12] and Arkansas total utilization rate of 35% in late 2021 placed it lowest in the country, below neighboring Mississippi (46.6%), Texas (49.6%), and Oklahoma (51.7%).[13] In response, SHARE led an effort to maximize value and the impact of WIC dollars for the highest-need Arkansans by cross-referencing data on Medicaid enrollment and relevant clinical-demographic indicators (postpartum status, children under age 5, A1C level, BMI) from its master patient index to identify potential WIC beneficiaries. Building on secure data flagging and patient matching processes that it used to connect ARHOME to providers and patients during the 2023 Medicaid redetermination process,[14] SHARE has successfully assisted ADH and Local Health Units with targeted outreach to eligible Medicaid beneficiaries and allow ADH staff to expedite their WIC enrollment.
Conclusion
The transformation of SHARE from a traditional Health Information Exchange (HIE) to a fully operational Health Data Utility (HDU) marks a watershed moment in Arkansas’ journey toward modernizing its public health infrastructure. This evolution is not merely a technological upgrade—it represents a strategic overhaul aimed at creating a dynamic, data-centric ecosystem that connects healthcare providers, public health agencies, and community services in unprecedented ways.
At its core, SHARE’s transition underscores the power of statewide interoperability. By linking diverse data systems and fostering public-private partnerships, Arkansas has built a robust framework that ensures critical health information is accessible and actionable. This seamless integration supports real-time data sharing across multiple sectors, allowing for rapid responses to public health emergencies and enhancing day-to-day care coordination. In practical terms, the digitization of registries and the enhanced integration of EMS data have filled longstanding gaps in data accessibility, resulting in more coordinated and efficient public health responses.
Moreover, SHARE’s forward-thinking approach extends beyond technical enhancements. Strategic initiatives, such as modernizing newborn screening protocols and streamlining disease surveillance, illustrate commitment to proactive, data-driven public health measures. By leveraging sophisticated analytics and targeted outreach strategies—such as those supporting WIC enrollments, SHARE is not only improving operational efficiency but also driving tangible improvements in population health outcomes and the health of Arkansans. These efforts underscore how advanced health data utilities can transform raw information into strategic insights that guide policy decisions and clinical practices.
Looking ahead, as SHARE continues to expand its capabilities and integrate even more deeply with public health and social services, it is setting a national benchmark for systemic modernization. Its holistic approach—combining advanced technology, strategic partnerships, and targeted public health initiatives—demonstrates the potential for HDU functionality to drive systemic change. By harnessing comprehensive data to inform decision-making, SHARE is helping to create a more resilient and responsive healthcare ecosystem, one that not only addresses immediate public health needs but also lays the groundwork for long-term improvements in care coordination and community well-being.
Learn more by visiting the SHARE website.
References:
[1] Arkansas Code Annotated. § 25-43-809. Office of Health Information Technology—Creation—Purpose—Policy. Available: A.C.A. § 25-43-809
[2] Arkansas Code Annotated. § 25-43-812. State Health Alliance for Records Exchange—Duties. Available: https://law.justia.com/codes/arkansas/title-25/chapter-43/subchapter-8/section-25-43-812/
[3] SHARE: State Health Alliance for Records Exchange. Available: https://sharearkansas.com/
[4] Office of the National Coordinator for Health IT. “Health IT State Summary—Arkansas.” 20 February 2015. Available: https://dashboard.healthit.gov/quickstats/widget/state-summaries/AR.pdf
[5] SHARE: State Health Alliance for Records Exchange. “What is SHARE.” Available: https://sharearkansas.com/about/about-share/
[6] SHARE: State Health Alliance for Records Exchange. “Which Providers are Using SHARE.” https://sharearkansas.com/our-progress/who-shares/
[7] SHARE: State Health Alliance for Records Exchange. “The Value of SHARE-ing Health Information.” 26 June 2024. Available: https://sharearkansas.com/2024/06/26/the-value-of-share-ing-health-information/
[8] Arkansas Department of Health. “Newborn Screening.” Available: https://healthy.arkansas.gov/programs-services/community-family-child-health/newborn-screening/
[9] Arkansas Department of Health. Data, Statistics, and Registries. Available: https://healthy.arkansas.gov/programs-services/data-statistics-registries/
[10] SHARE: State Health Alliance for Records Exchange. “UAMS IDHI Brain Injury Program Emphasizes Value of SHARE Hospitalization Alerts: Raising the Quality of Care While Providing Long-Term Care.” Available: https://sharearkansas.com/2024/05/20/uams-idhi-brain-injury-program-emphasize-value-of-share-hospitalization-alerts-raising-the-quality-of-care-while-providing-long-term-care/
[11] USDA Food and Nutrition Service. “WIC Eligibility Requirements—Am I Eligible.” Available: https://www.fns.usda.gov/wic/applicant-participant/eligibility#:~:text
[12] Neuberger, Zoe. “WIC Coordination with Medicaid and SNAP.” Center on Budget and Policy Priorities. 8 October 2024. Available: https://www.cbpp.org/research/food-assistance/wic-coordination-with-medicaid-and-snap-1
[13] USDA Food and Nutrition Service. “National and State-Level Estimates of WIC Eligibility and Program Reach in 2021.” Available: https://www.fns.usda.gov/research/wic/eligibility-and-program-reach-estimates-2021
[14] SHARE: State Health Alliance for Records Exchange. “A Newsletter from SHARE—Spring 2023.” Available: https://sharearkansas.com/wp-content/uploads/Spring-2023-SHARE-Newsletter.pdf
February 2025 Network News
February Network News
Thank you to everyone who joined us for the February 2025 Network News where we heard from our new Board of Director Officers about their interest in serving on the Civitas Board and goals for Civitas in 2025 and beyond.
If you want a refresher or if you couldn’t make it to the live event, please check out the recording and presentation slides linked below.
For those curious about how to make the most of your Civitas membership this year, please check out our recent blog post.
Civitas at HIMSS25
Civitas Networks for Health is proud to collaborate with HIMSS for their highly anticipated #HIMSS25 Global Health Conference in Las Vegas. Taking place from March 3-6, 2025, this event is the epicenter of health care innovation, bringing together industry leaders, innovators, and professionals from across the digital health ecosystem to advance health IT and interoperability.
What Makes HIMSS25 Unique?
- Cutting-Edge Educational Opportunities: Delve into a diverse array of sessions led by expert speakers, covering key topics such as digital health transformation, data governance, health equity, AI-driven patient care, and more. Attendees can also earn CE credits to stay ahead of industry trends.
- Innovative Pavilions and Forums: Experience groundbreaking exhibits like the AI Pavilion, Interop+Smart Experience Pavilion, and First-Time Exhibitors Pavilion. New preconference forums, including the Health Equity and Smart Health Transformation forums, will provide actionable strategies to tackle pressing challenges in health IT.
- Showcasing Emerging Talent: The Emerge Innovation Experience offers a platform for startups and innovators to showcase breakthrough ideas, making it a must-visit for investors and early adopters.
- Emerging Healthcare Leaders Reception – HIMSS Health Conference & Exhibition: The HIMSS team is hosting an exciting evening reception where you can mix and mingle with other vibrant young professionals. Enjoy awesome music, delicious food, creative dessert drinks, and great company! Learn more.
- Exclusive Networking Opportunities: Engage with health care professionals, including Civitas members, to discuss how local networks fuel national transformation. Civitas is hosting a member meetup on March 4 at 4:00 PM, co-hosted with InterSystems.
Want to learn more? Check out everything new at HIMSS25 by visiting the HIMSS website.
Civitas members can access exclusive discounts. For details, email contact@civitasforhealth.org and ask about your HIMSS registration discount code.
Civitas Involvement at HIMSS25 and Interesting Conversations We're Looking Forward To
Civitas Networks for Health is proud to have a role in shaping conversations at HIMSS25. From moderating dynamic discussions on interoperability to hosting a dedicated member meetup, Civitas is fostering collaboration and furthering the national dialogue on how we are using data to drive health system transformation.
Here are a few things to look forward to at the conference:
Real Discussions on Advanced Interoperability – Breakthroughs & Barriers
"The State of Interoperability & HIE Today" opening keynote will set the stage for a day of deep discussions on the breakthroughs and barriers in healthcare data exchange. Taking place on Monday, March 3, at 8:30 AM (PT) as part of the Interoperability & HIE Preconference Forum, this keynote will provide a high-level overview of the current interoperability landscape, highlighting both progress and persistent challenges. Brendan Keeler, Interoperability and Data Liquidity Practice Lead at HTD Health, will explore evolving standards, policy impacts such as the 21st Century Cures Act and Information Blocking Rules, and the role of HIEs in improving care coordination and patient outcomes. This session will offer valuable insights for health IT leaders, policymakers, and interoperability advocates navigating the complex and ever-changing health data ecosystem. Additional registration is required to attend this exclusive forum, making it a must-attend event for those driving forward interoperability efforts in 2025 and beyond.
Additionally, Civitas CEO Lisa Bari will moderate two sessions as part of the Interoperability and HIE Forum (preconference) on March 3, 2025, at the Venetian Hotel. The Forum sessions will tackle critical topics, including privacy, regulatory frameworks, and the evolving landscape of the Trusted Exchange Framework and Common Agreement (TEFCA). Civitas is proud to have served on the HIE and Interoperability Forum Committee helping to bring attention to pressing topics and in designing meaningful programming.
Forum highlights included:
- Opening Keynote: A powerful overview of the current state of interoperability, featuring recent advancements, persistent barriers, and the opportunities ahead.
- Fireside Chat: Industry leaders discuss real-world success stories, lessons learned, and policy impacts on interoperability efforts.
- Audience Reactor Roundtable: An interactive session encouraging audience dialogue on strategies to advance interoperability initiatives.
Here are the details for the two sessions Lisa will moderate – mark your calendars:
Fireside Chat - The State of Interoperability & HIE Today: Breakthroughs & Barriers
- Monday, March 3, 2025, 9:05 AM to 9:50 AM · 45 min. (US/Pacific)
- Venetian | Level 3 | Lido 3101
Crowd Pulse: The Audience Reactor Roundtable - The State of Interoperability & HIE Today
- Monday, March 3, 2025, 9:50 AM to 10:15 AM · 25 min. (US/Pacific)
- Venetian | Level 3 | Lido 3101
Civitas Member Meetup at HIMSS 2025
Join Civitas and our member co-hosts, InterSystems, for an exclusive member meetup on Tuesday, March 4, from 4:00 –5:30 PM. This is your chance to connect with peers, share insights, and deepen relationships with other Civitas members .
For event details, email contact@civitasforhealth.org.
Civitas Member and Partner Sessions at HIMSS 2025
| Session Title | Time, Location | Featured Civitas Member(s)/Partners |
| March 3, 2025 | ||
| The State of Interoperability & HIE Today: Breakthroughs & Barriers | 9:05 AM to 9:50 AM PT
Venetian | Level 3 | Lido 3101 |
eHealth Exchange
Medica |
| Crowd Pulse: The State of Interoperability & HIE Today | 9:50 AM to 10:15 AM
Venetian | Level 3 | Lido 3101 |
eHealth Exchange
Medica
|
| Advancing Public Health with Interoperable Data | 10:25 AM to 10:55 AM
Venetian | Level 3 | Lido 3101 |
Chicago Region-Wide CIE/Illinois Public Health Institute |
| What’s SOP with TEFECA & QHINs? | 11:00 AM to 12:00 PM
Venetian | Level 3 | Lido 3101 |
KONZA National Network |
| What's Happening on the Ground: Real-World Evidence and State-Level Data Initiatives | 11:00 AM to 12:00 PM PT
Venetian | Level 5 | Palazzo M |
EMI Advisors
N.C. Health Information Exchange Authority |
| The Role of Next-Gen Health Data Networks | 1:00 PM to 1:45 PM
Venetian | Level 3 | Lido 3101 |
CRISP & CRISP Shared Services
Velatura Health Information Exchange Corporation |
| Payers’ Use of Interoperable Data: Improving Member Experience & Outcomes | 3:30 PM to 4:00 PM
Venetian | Level 3 | Lido 3101 |
BlueCross BlueShield Association |
| March 4, 2025 | ||
| ED & Post-Acute Collaboration: Streamlining SNF Transfers with Real-Time Data | 12:45 PM to 1:45 PM
Venetian | Level 3 | San Polo 3501 |
PointClickCare |
| Interoperability, AI, and Digital Health: Nordic-US Learnings and Perspectives on What’s Next | 3:00 PM to 5:00 PM
Venetian | Level 4 | Delfino 4103 |
InterSystems |
| HIMSS (Latin America) LATAM Summit | 1:30 PM to 4:30 PM
Venetian | Level 5 | Palazzo E |
InterSystems |
| The Rationalization of Resilience: Why Uptime is of Utmost Importance in Healthcare | 3:15 PM to 4:15 PM
Venetian | Level 3 | San Polo 3501 |
Amazon Web Services, Inc. |
| State-Level Public Health and the Journey Toward Digital Maturity | 2:00 PM to 3:00 PM
Caesars | Forum 123 |
Guidehouse (Partners of Civitas) |
| Cross-Cabinet Effort: Unlocking Healthcare Data for Child Welfare | 3:15 PM to 4:15 PM
Venetian | Level 2 | Veronese 2501 |
Deloitte |
| March 5, 2025 | ||
| Interoperability: Fueling Digital Health Innovation with Data | 10:00 AM to 11:00 AM
Venetian | Level 3 | San Polo 3501 |
InterSystems |
| International Workshop: From Innovation to Integration- Practical Considerations for Clinical AI | 1:30 PM to 3:00 PM
Venetian | Level 4 | Delfino 4103 |
InterSystems |
| HIMSS Brazil Summit | 1:30 PM to 4:30 PM
Venetian | Level 5 | Palazzo E |
InterSystems |
| Achieving Clinical and Operational Excellence with a Modern Data Platform powered by AWS | 4:00 PM to 4:30 PM
Main Stage |
Amazon Web Services |
| March 6, 2025 | ||
| Advancing Consensus-Driven Standards to Support Social Determinants of Health | 8:30 AM to 9:30 AM | 211 San Diego |
| AI Transforming Healthcare: Real-World Evidence & Clinical Impact in Pediatric Care | 9:45 AM to 10:45 AM
Venetian | Level 2 | Venetian F |
Amazon Web Services |
| How UK & Ireland Health Systems Achieve Digital Maturity: Adopting the Right Tech, at the Right Scale, for the Right People | 10:30 AM to 12:30 PM
Venetian | Level 4 | Delfino 4103 |
InterSystems |
| Leveraging Conversational AI to Drastically Reduce Payer Denials | 12:45 PM to 1:45 PM
Venetian | Level 3 | Lido 3104 |
Guidehouse (Partners of Civitas) |
| Building Digitally Enabled Air Traffic Control Model for Crisi Services | 2:00 PM to 3:00 PM
Caesars | Forum 116 |
Contexture |
| HIE and Criminal Justice Partnership Impact on Whole-Person Health | 2:00 PM to 3:00 PM
Caesars | Academy 415 |
Contexture |
If we missed your organization in the lineup, let us know so we can add you!
Civitas’ Commitment to Health and Health Care Transformation
Civitas proudly represents a diverse network of organizations—including Health Information Exchanges (HIEs), Community Information Exchanges (CIEs), Health Data Utilities (HDUs), All Payer Claims Databases (APCDs), Regional Health Improvement Collaboratives (RHICs), and Quality Improvement Organizations (QIOs) among other strategic business and technology partners—working together to transform health care through data-led collaboration. HIMSS25 offers a platform to highlight how these partnerships and local networks drive national impact, from enhancing care coordination to advancing interoperability.
Civitas is excited to be at the event and encourages you to join us in Las Vegas as we build a more sustainable, equitable, and connected health system.
For more information on HIMSS25 and Civitas events, visit HIMSS25 Website or contact us at contact@civitasforhealth.org.











